Haemophilia
Haemophilia is a rare but serious blood disorder that prevents proper blood clotting. People with this condition need medical treatment throughout their lives. The condition's effects range from mild to severe cases, and the severity depends on blood clotting factor levels.
People with this condition bruise easily and bleed more than normal after injuries or surgeries. Most symptoms show up during early childhood, though some cases remain undetected until later.
Many people still don't understand how this condition disrupts daily life. This article covers everything from symptoms and causes to diagnosis and cures for haemophilia that help people manage this challenging blood disorder.
What is Haemophilia?
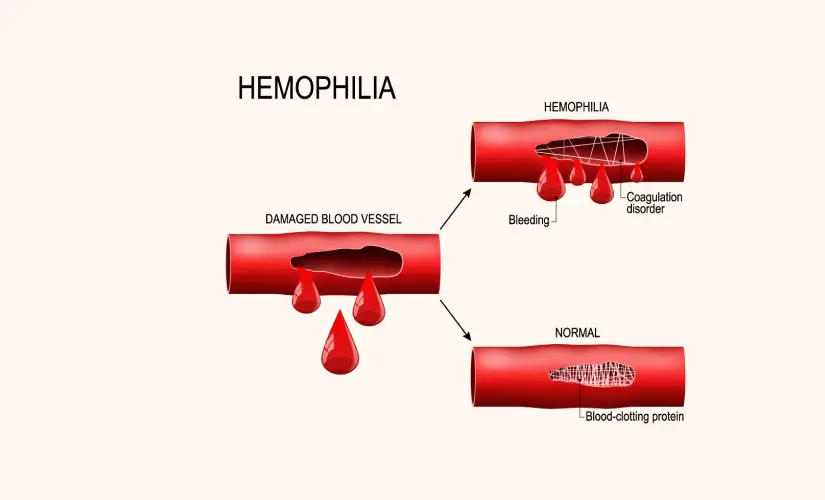
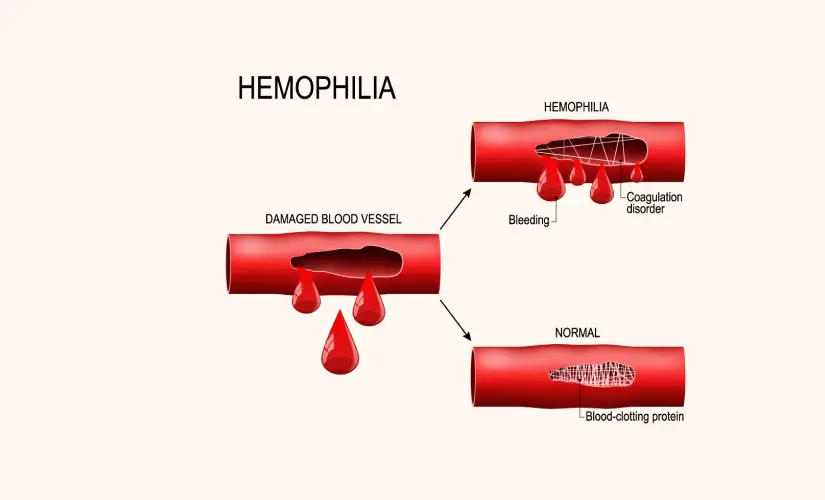
People with haemophilia have blood that doesn't clot properly because they lack certain clotting factors. Blood contains proteins called clotting factors that help stop bleeding. The following are common types of haemophilia:
- Haemophilia A affects one in every 4,000-5,000 males worldwide and occurs when levels of factor VIII are too low.
- Haemophilia B develops when factor IX levels are too low.
- There is also a rare type called haemophilia C that happens due to factor XI deficiency.
Symptoms of Haemophilia
Excessive bleeding that won't stop easily is the most important sign. Other haemophilia symptoms are:
- Joint bleeding with swelling, pain, and tightness, especially in the knees, elbows, and ankles
- Big bruises from small injuries
- Extended bleeding after losing teeth, getting vaccinations, or having surgery
- Blood appearing in urine or stool
- Frequent nosebleeds
The amount of clotting factor in blood determines how severe the symptoms become.
Haemophilia Causes
Gene mutations on the X chromosome typically cause haemophilia. Males inherit the disease if they get the affected gene because they have just one X chromosome. Women who have one affected X chromosome usually become carriers. Their second X chromosome protects them from showing symptoms. About one-third of babies diagnosed with haemophilia have no other family members with the condition. The immune system sometimes creates antibodies against clotting factors which leads to acquired haemophilia in rare cases.
Risk Factors
These factors increase the chance of developing haemophilia:
- A family's history of bleeding disorders
- The male gender because of X-linked inheritance
- Mother carrying the haemophilia gene
- Medical conditions like pregnancy, autoimmune disorders, cancer, or medication interactions can cause acquired haemophilia.
Complications of Haemophilia
Haemophilia can cause serious problems if not managed properly:
- Repeated bleeding damages joints and leads to chronic arthritis and disability
- The body might develop inhibitors against replacement clotting factors
- Blood pools called pseudotumors form near bones
- Brain bleeding can cause neurological damage
- Pressure on the arteries and nerves results in compartment syndrome
Diagnosis
Blood tests are the first step doctors take to detect haemophilia. These tests measure clotting factor levels and determine how severe the condition is. The diagnostic process includes:
- CBC tests to assess overall blood health
- APTT tests showing slower clotting in haemophilia
- PT tests that typically indicate normal results
- Specific factor assays verify haemophilia type and find the missing factor.
Doctors classify severity based on clotting factor percentage: mild (5-40%), moderate (1-5%), or severe (less than 1%).
Haemophilia Treatment
The primary focus of haemophilia care is clotting factor replacement. Each patient needs a customised treatment plan:
- Factor VIII replacement therapy for haemophilia A
- Factor IX replacement therapy for Haemophilia B
- In less severe cases medicines like desmopressin (DDAVP) help release clotting factors.
- Modern therapies include emicizumab, which mimics factor VIII function.
- Gene therapy approaches have gained approval for adults with specific forms.
Patients with severe haemophilia need regular prophylactic factor injections—up to three times weekly—to prevent bleeding.
When to See a Doctor
Contact your doctor if you experience:
- Joint or muscle pain with swelling, tingling, or numbness
- Blood appearing in urine or stool
- Bleeding that won't stop
- Head injuries, sudden severe headaches, or major injuries require immediate emergency care.
Conclusion
Living with haemophilia brings unique challenges, but modern treatments give hope and improve quality of life by a lot compared to previous generations. People with this blood disorder have several options to manage their condition. Regular factor replacement helps many patients to live normal lives even with clotting issues.
Families dealing with haemophilia need proper education. Quick recognition of symptoms helps detect bleeding episodes early. Knowledge of emergency procedures can save lives. Support groups are a great way to get an emotional connection with others who face similar challenges.
Medical advances continue to change haemophilia care. Gene therapy looks promising as researchers strive to find cures instead of just managing symptoms. For now, care teams help patients create tailored treatment plans based on their condition type and severity. With the right medical care, people with haemophilia live active lives and handle their condition well.
FAQs
1. What are three symptoms of haemophilia?
The following are primary symptoms:
- Joint bleeding - Your knees, elbows, and ankles might feel painful, swollen and tight
- Easy bruising - You will notice large bruises even after small accidents
- Prolonged bleeding - Blood doesn't clot easily after injuries, dental work, or surgery
2. Who is at risk for haemophilia?
Males face the highest risk of haemophilia. The genetic mutations that cause this condition live on the X chromosome. Men have XY chromosomes, so they develop haemophilia when they inherit the altered gene. They lack another X chromosome to make up for it. Women usually become carriers without symptoms. About one-third of female carriers show bleeding symptoms.
3. How to prevent haemophilia?
No one can prevent haemophilia because it's genetic. People with this blood disorder can reduce bleeding episodes with these steps:
- Stay away from contact sports and high-impact activities
- Use protective gear during physical activities
- Keep your teeth and gums healthy
- Check with your doctor before taking blood-thinning medicines like aspirin
- Get all recommended vaccines
4. What are the first signs of haemophilia?
Babies might show early signs of haemophilia. Excessive bleeding can happen after heel sticks, circumcision or birth trauma. Unexplained bruising becomes obvious when children start moving around at 12-18 months. Watch for bleeding in the mouth, especially near the gums or after losing teeth. Frequent nosebleeds that won't stop easily need attention too.