-
Doctors
-
Specialities & Treatments
Centre of Excellence
Specialties
Treatments and Procedures
Hospitals & Directions HyderabadCARE Hospitals, Banjara Hills CARE Outpatient Centre, Banjara Hills CARE Hospitals, HITEC City CARE Hospitals, Nampally Gurunanak CARE Hospitals, Musheerabad CARE Hospitals Outpatient Centre, HITEC City CARE Hospitals, Malakpet
HyderabadCARE Hospitals, Banjara Hills CARE Outpatient Centre, Banjara Hills CARE Hospitals, HITEC City CARE Hospitals, Nampally Gurunanak CARE Hospitals, Musheerabad CARE Hospitals Outpatient Centre, HITEC City CARE Hospitals, Malakpet Raipur
Raipur
 Bhubaneswar
Bhubaneswar Visakhapatnam
Visakhapatnam
 Nagpur
Nagpur
 Indore
Indore
 Chh. Sambhajinagar
Chh. SambhajinagarClinics & Medical Centers
Book an AppointmentContact Us
Online Lab Reports
Book an Appointment
Consult Super-Specialist Doctors at CARE Hospitals

Osteomalacia
Symptom, Causes, Diagnosis and Treatment
Osteomalacia
Vitamin D deficiency stands as the world's most widespread nutritional deficiency, but people rarely understand its dangerous effects. This deficiency leads to osteomalacia, which doctors call "soft bone disease," and it weakens the bone structure significantly.
The condition causes bone pain that patients feel in their legs, groin, upper thighs and knees. Low levels of vitamin D, calcium, or phosphate in the body trigger this painful condition. Food fortification with vitamin D almost eliminated rickets (the childhood version) in Western countries during the early 20th century. However, doctors have noticed a troubling increase in cases over the last several years. Undiagnosed osteomalacia can result in broken bones and severe deformity. The condition makes walking a challenge because of painful partial fractures that doctors call Looser's zone.
What is Osteomalacia?
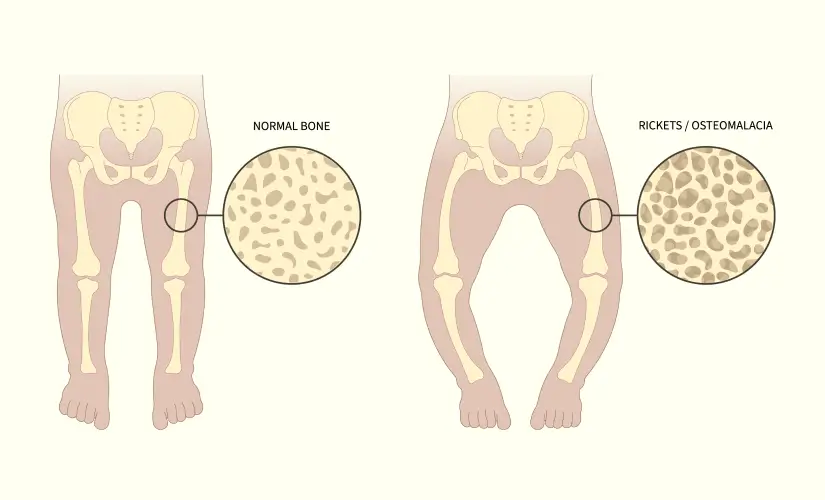
Adults can develop soft bones, a condition known as osteomalacia. This condition differs from osteoporosis, which thins the bones. Osteomalacia occurs because bones fail to mineralise properly. Your bones become weak and soft and might bend under pressure. The term actually means "soft bones," which perfectly describes this disorder's nature.
Symptoms of Osteomalacia
People might not notice any osteomalacia symptoms during the early stages. The condition progresses and shows these symptoms:
- Your bones hurt, especially in the hips, pelvis, legs and lower back, and the pain gets worse with movement
- Weak muscles make it hard to climb stairs
- Walking becomes difficult with a distinctive waddle
- Bones feel tender to touch
- Minor bumps or falls can cause bone fractures
- Hands and feet experience pins and needles sensations
The weakness mainly affects your thighs, shoulders and trunk. Simple movements become painful, and resting helps reduce discomfort.
Causes of Osteomalacia
Vitamin D deficiency stands out as the main cause. Your body has to have vitamin D to absorb calcium and phosphorus - these minerals build strong bones. Bones can't mineralise properly without enough vitamin D.
Several other factors can cause osteomalacia:
- Celiac disease and other digestive problems
- Problems with the kidneys or liver
- Some medications, especially anti-seizure drugs
- Low phosphate levels
Risks of Osteomalacia
The condition affects certain groups more:
- People with minimal sun exposure
- Residents of cold, dark climates
- Those with darker skin
- People following vegetarian or vegan diets
- Adults over 65
- Pregnant and breastfeeding women
- People who cover most of their skin with clothing
Complications of Osteomalacia
Untreated osteomalacia can result in:
- Partial fractures called Looser's zones
- Complete bone fractures
- Lasting bone deformities, including a curved spine
- Long-term movement problems
The good news is that most patients respond well to treatment and can expect positive results.
Diagnosis
Doctors start by getting into your medical history and conducting physical tests. Blood tests provide vital information about:
- Vitamin D, calcium and phosphate levels
- Alkaline phosphatase (typically elevated)
- Parathyroid hormone (often increased)
- Creatinine and electrolytes
X-rays detect pseudofractures (also called Looser zones), and bone density scans reveal bone loss patterns. These scans might show osteomalacia looking similar to osteoporosis, but these conditions are fundamentally different. Doctors might recommend a bone biopsy in unclear cases - the gold standard for diagnosis.
Treatments for Osteomalacia
The primary focus of osteomalacia treatment plans is to restore vitamin D levels. Common approaches include:
Doctors usually prescribe daily vitamin D supplements, starting with higher doses (50,000 IU weekly for 8-12 weeks) before moving to maintenance doses of 800-2000 IU daily.
Calcium supplements (1000 mg daily) work alongside vitamin D therapy. Patients with absorption problems might need higher doses or special vitamin D forms.
Most patients see improvements within weeks, though complete healing takes several months. Regular blood tests help monitor progress during treatment.
When to See a Doctor
You should reach out to doctors right away if you experience:
- Persistent bone pain or muscle weakness
- Difficulty walking
- Unexplained fractures
- Pain when bones are touched
Prevention
Sunlight exposure is a great way to get natural vitamin D - just 10-15 minutes of midday sun several times weekly helps most people. Your body also benefits from foods rich in vitamin D (fatty fish, egg yolks, fortified products) and calcium.
People at higher risk should think about daily supplements after talking to their doctors. A healthy weight, avoiding smoking, and moderate alcohol consumption help protect your bone strength.
Conclusion
Millions of people worldwide suffer from osteomalacia, yet it often goes unnoticed. Your bones might soften slowly over time, but most patients can make a full recovery with the right diagnosis. Blood tests, X-rays, and physical examinations help doctors spot this condition, though getting diagnosed can take years.
Vitamin D plays a vital part in keeping your bones healthy. People who live nowhere near the equator have a higher risk, as do those with darker skin or who keep most of their body covered. Older adults and pregnant women should pay special attention to their bone health.
The treatment success rate is remarkable. Most patients start feeling better just weeks after beginning vitamin D and calcium supplements. While complete recovery takes time, bones generally become stronger with consistent treatment.
Getting ahead of bone problems works better than treating them, without a doubt. Your body makes its own vitamin D when you spend short periods in the sun a few times each week. On top of that, eating fatty fish, eggs, and fortified foods helps boost your levels naturally. Regular doctor visits are important, especially if you notice unexplained bone pain or weakness.
FAQs
1. What are the leading causes of osteomalacia?
Vitamin D deficiency is the most important reason behind osteomalacia cases. Here are other reasons why it happens:
- Digestive disorders - Celiac disease, Crohn's disease, and cystic fibrosis prevent proper nutrient absorption
- Kidney or liver problems - These organs help activate vitamin D, which reduces bone-strengthening abilities when damaged
- Medication effects - Anti-seizure drugs (phenytoin, carbamazepine), rifampin, and some antacids interfere with vitamin D processing
- Limited sunlight exposure - The risk increases for people living in northern climates or those spending little or no time outdoors
- Dietary factors - Low calcium intake can trigger osteomalacia even with enough vitamin D
Genetic disorders affecting phosphate metabolism and tumour-induced conditions that alter the body's mineral balance are rare causes.
2. What vitamin deficiency causes osteomalacia?
Vitamin D deficiency is the basic nutritional gap that leads to osteomalacia. This vital vitamin comes from:
- Sunlight exposure on the skin (main natural source)
- Dietary sources (fatty fish, egg yolks, and fortified foods)
- Supplements (often needed for treatment)
Still Have a Question?