-
Doctors
-
Specialities & Treatments
Centre of Excellence
Specialties
Treatments and Procedures
Hospitals & Directions HyderabadCARE Hospitals, Banjara Hills CARE Outpatient Centre, Banjara Hills CARE Hospitals, HITEC City CARE Hospitals, Nampally Gurunanak CARE Hospitals, Musheerabad CARE Hospitals Outpatient Centre, HITEC City CARE Hospitals, Malakpet
HyderabadCARE Hospitals, Banjara Hills CARE Outpatient Centre, Banjara Hills CARE Hospitals, HITEC City CARE Hospitals, Nampally Gurunanak CARE Hospitals, Musheerabad CARE Hospitals Outpatient Centre, HITEC City CARE Hospitals, Malakpet Raipur
Raipur
 Bhubaneswar
Bhubaneswar Visakhapatnam
Visakhapatnam
 Nagpur
Nagpur
 Indore
Indore
 Chh. Sambhajinagar
Chh. SambhajinagarClinics & Medical Centers
Book an AppointmentContact Us
Online Lab Reports
Book an Appointment
Consult Super-Specialist Doctors at CARE Hospitals

High Eosinophils
Symptom, Causes, Diagnosis and Treatment
High Eosinophils
Eosinophilia is a disorder in which our body creates an abnormally large number of eosinophils, a type of white blood cells (WBC). These white blood cells are crucial for the immune system's defense against diseases and infections. The eosinophil count can help doctors determine if someone has an underlying medical disease, such as an autoimmune disorder, or whether their body is only battling allergies or an infection. Very rarely, elevated eosinophil levels might be caused by particular medical conditions and medications.
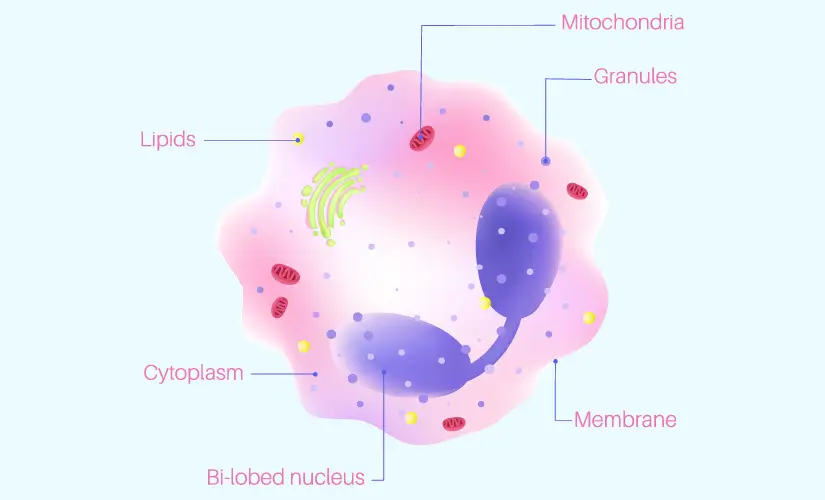
Definition of Eosinophils
Eosinophils are a type of disease-fighting white blood cell. They are produced by the bone marrow and then migrate to various tissues. They assist our body in protecting itself from fungal infections, viral infections, bacterial infections, and parasites, such as worms.
Eosinophils typically makeup 0.5–1% of all white blood cells in humans and seldom exceed 5% of all white blood cells. Eosinophil count in healthy individuals is under 500 cells per microliter (cells/mcL). A count is considered high if it exceeds 500 cells per microliter of blood and low if it is fewer than 30 cells per microliter of blood. Eosinophil levels change with age in children.
Eosinophilia is categorized by doctors into one of three groups. These consist of:
- mild (500–1,500 eosinophil cells per mL)
- moderate (1,500–5,000 eosinophil cells per mL)
- severe (greater than 5,000 eosinophil cells per mL)
Causes of High Eosinophils
Eosinophilia is frequently associated with a range of diseases. An elevated eosinophil count might result from:
- Fungal infections
- Adrenal gland deficiency
- Various blood-related conditions, including leukemia
- Autoimmune diseases
- Eczema
- Cancerous tumors
- Infection from parasites, such as worms
- Allergy-related diseases, such as hay fever
- Hypereosinophilic syndrome
- Leukemia and other blood disorders
- Lymphoma
- Asthma
- Upper respiratory diseases, such as rhinitis
Other Potential Causes
Eosinophilia can be attributed to a variety of diseases:
- Seasonal allergies and medication reactions are two examples of frequently occurring conditions, which are generally not very dangerous
- Certain medications
- Blood cancers
- Genetic mutations
A lower-than-average eosinophil count might result from:
- Effects of Alcohol
- Body's overproduction of some steroids (such as cortisol)
Symptoms and Signs of High Eosinophils
The symptoms of high eosinophil count include:
- Rash
- Itching
- Diarrhea in the event of parasite infections
- Asthma
- Runny nose, especially if it's connected to allergies
- Chronic eosinophilic cough
Medical Conditions Associated with High Eosinophils
In certain situations, eosinophils cause inflammation in particular parts of the body. When this happens, the condition is known as an eosinophilic disorder or hypereosinophilic syndrome (HES), where it can affect the bladder, skin, lungs, heart, etc. Some other conditions associated with high eosinophil count are:
- Eosinophilic cystitis: It is a bladder condition.
- Eosinophilic pneumonia: This medical condition affects your lungs.
- Eosinophilic fasciitis: This is a condition of the fascia, the connective tissue that runs throughout the body.
- Eosinophilic gastrointestinal disorders (EGID): Eosinophilic esophagitis and conditions that affect your colon (large intestine), stomach, and small intestine are all included in EGID.
- Eosinophilic granulomatosis with polyangiitis (EGPA): This disease, sometimes referred to as Churg-Strauss syndrome, affects your heart, lungs, and other organs.
Diagnostic Tests for High Eosinophils
Most of the time, high eosinophils are identified by medical professionals during a normal blood test called a complete blood count (CBC) with a differential white blood cell count. A high level of eosinophils in blood test can determine the levels of eosinophils in the peripheral blood. However, there are additional tests to consider to know the severity of the condition:
- Liver function tests
- Urine tests
- Stool sample testing
- Additional blood tests
- Chest X-rays
- Tissue and bone marrow biopsies
If a medication is the cause of eosinophilia, there may not be a specific test to identify it. It is generally assumed that the medication was the source of the problem if the eosinophil count returns to normal after stopping the prescription. Stool samples are collected and tested to identify various parasite infestations.
Treatment of High Eosinophils
Generally, eosinophil count can be corrected by treating the underlying condition or the actual cause.
- If the cause of high eosinophil count is certain medications or foods, the doctor advises you to stop using them.
- If the patient has chronic sinusitis or allergies that are the cause of high eosinophils in blood, the doctor may recommend allergy testing to identify the allergens that triggered the allergic reaction.
- The doctor will address any existing infections if a certain infection is the cause.
- If the cause is blood cancer, it will be treated by the doctor accordingly.
Prevention of High Eosinophils
Allergy-related eosinophilia can be addressed by using medication to reduce the body's allergic responses. However, there are times when eosinophilia might be an indication of a serious underlying medical condition that must be avoided. The occurrence of eosinophilia can be decreased by taking certain precautions, such as -
- Avoid raw fish, meat, snails, prawns, and other seafood.
- Wash fruit and vegetables thoroughly to get rid of parasites.
- Keep your surroundings clean.
- Avoid medications you are allergic to.
Importance of Timely Diagnosis and Treatment
A delay in referral and treatment for a high eosinophil count may have significant negative effects on the progression of the patient's condition. Therefore, it is crucial to identify the specific type and cause of high eosinophils. Timely diagnosis and treatment are critically important in healthcare for several reasons. Here are some key aspects highlighting the significance of promptly identifying and addressing medical conditions:
- Improved Outcomes: Early diagnosis and intervention often lead to better treatment outcomes. Identifying a health issue in its early stages allows for more effective and less aggressive treatment, reducing the risk of complications and improving the chances of a positive outcome.
- Prevention of Progression: Many medical conditions, if left untreated, can progress and become more severe over time. Early diagnosis allows healthcare providers to intervene before the condition advances, preventing complications and irreversible damage.
- Enhanced Quality of Life: Timely treatment can alleviate symptoms, improve overall well-being, and enhance the quality of life for individuals with health conditions. Managing a condition in its early stages often results in a better quality of life compared to dealing with advanced or chronic illnesses.
- Reduced Healthcare Costs: Addressing health issues early can help reduce healthcare costs. Preventing the progression of a condition to more advanced stages may require fewer medical interventions, hospitalizations, and long-term medications.
- Prevention of Spread of Infectious Diseases: Timely diagnosis and treatment of infectious diseases are crucial for preventing the spread of illnesses within communities. Early identification allows for prompt implementation of isolation measures, contact tracing, and appropriate medical interventions to contain the disease.
- Minimized Complications: Early intervention can prevent or minimize complications associated with various health conditions. Complications are often more challenging to manage and may have long-term consequences for an individual's health.
- Patient Empowerment: Timely diagnosis provides patients with the information they need to actively participate in their healthcare decisions. It empowers individuals to make informed choices about their treatment options and lifestyle modifications.
Conclusion
Generally, a high eosinophil count is not a cause for immediate concern. However, the doctor may recommend further testing to determine the implications of a high eosinophil count. Once the underlying cause of eosinophilia has been identified, the doctor will provide treatment.
FAQs
1. What is considered a high eosinophil count?
In adults, eosinophilia is often defined as a blood count of 500 or more eosinophils per microliter. A high eosinophil range is defined as an eosinophil count above 1,500 cells per microliter of blood that lasts for several months. The normal range for eosinophils in percentage is 1 to 6 % of the blood.
2. Can high eosinophils be a sign of allergies?
High eosinophil levels may indicate a minor illness, such as an allergic reaction to a medication, or a more serious condition, such as various blood disorders.
3. Are there any specific medical conditions associated with high eosinophils?
Blood or tissue eosinophilia can be caused by several specific diseases and disorders, including:
- Myelogenous thrombocytopenic purpura (MTP)
- Allergies
- Roundworm infection is known as ascariasis
4. Can high eosinophils lead to complications?
Eosinophils can occasionally cause inflammation in specific parts of the body. This condition is referred to as eosinophilic disorders or hypereosinophilic syndrome (HES). Eosinophilia can result in damage to end organs, potentially affecting any organ in the body.

Still Have a Question?



