-
Doctors
-
Specialities & Treatments
Centre of Excellence
Specialties
Treatments and Procedures
Hospitals & Directions HyderabadCARE Hospitals, Banjara Hills CARE Outpatient Centre, Banjara Hills CARE Hospitals, HITEC City CARE Hospitals, Nampally Gurunanak CARE Hospitals, Musheerabad CARE Hospitals Outpatient Centre, HITEC City CARE Hospitals, Malakpet
HyderabadCARE Hospitals, Banjara Hills CARE Outpatient Centre, Banjara Hills CARE Hospitals, HITEC City CARE Hospitals, Nampally Gurunanak CARE Hospitals, Musheerabad CARE Hospitals Outpatient Centre, HITEC City CARE Hospitals, Malakpet Raipur
Raipur
 Bhubaneswar
Bhubaneswar Visakhapatnam
Visakhapatnam
 Nagpur
Nagpur
 Indore
Indore
 Chh. Sambhajinagar
Chh. SambhajinagarClinics & Medical Centers
Book an AppointmentContact Us
Online Lab Reports
Book an Appointment
Consult Super-Specialist Doctors at CARE Hospitals

Aortic Arch Disease
Aortic Arch Disease
Aortic Arch Syndrome Treatment in Hyderabad, India
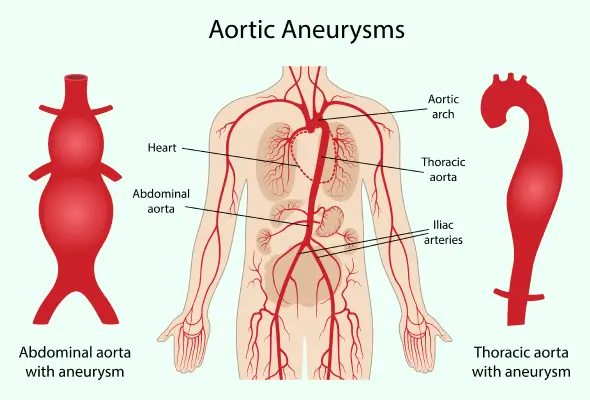
The Aorta is the largest blood vessel in the body. The blood flow runs from the heart, through the chest, and into the abdomen. Aortic arch conditions affect the arteries that branch off the top of the aorta. They can decrease blood flow to essential organs.
The doctors at CARE Hospitals specialize in diagnosing and treating diseases affecting the arterial, venous, and lymphatic systems outside of the heart and brain. We provide comprehensive vascular care made possible by state-of-the-art technology. We focus on perfecting Aortic Arch Disease Treatment Cost in Hyderabad.
Takayasu’s arteritis, an autoimmune disorder that inflames the aorta and pulmonary arteries (which supply the lungs with blood), can cause aortic arch disease. Blood pressure changes, clots, trauma, a congenital disorder, or Takayasu’s arthritis can all cause the condition. Asian females tend to catch Takayasu's between ages 10 and 30.
Eventually, the blood vessels that branch off the aorta become blocked, decreasing blood flow throughout the body. As the arteries narrow, the blood flow is reduced, and the arteries weaken, an aneurysm, or abnormal bulge, develops in the wall of the arteries. An aneurysm can rupture and pose a serious risk to a person’s life. The most common cause of aortic arch disease is atherosclerosis or the hardening of the arteries.
Symptoms and signs
The aortic arch syndrome symptoms are diverse and depend heavily on the disease's stage and which blood vessels are affected. In the earlier inflammatory stage, individuals may experience general flu-like symptoms, fatigue, and joint pain. However, as the disease progresses to the occlusive stage and blood vessels begin to narrow, more specific symptoms emerge.
The first phase of the disease is marked by the following symptoms occurring in approximately half of all patients:
-
Fever
-
Fatigue
-
Poor appetite
-
Weight loss
-
Night sweats
-
Joint pain
-
Chest pain
-
Muscle aches
-
Swollen glands
-
Tenderness above the affected arteries.
Symptoms of an occlusive phase include:
-
Fatigue
-
Muscle weakness
-
Pain
-
Cramping
-
Nausea
-
Vomiting
-
Cold or white hands or feet
-
High blood pressure
-
Weak or absent pulse
-
Vision problems
-
A difference in blood pressure between the arms and the legs.
During the occlusive phase of the disease, other serious conditions can occur. The conditions include hypertension, renal (kidney) failure, anginal (chest pain), congestive heart failure, transient ischemic attack (or mini-stroke), and stroke.
Diagnosis
Diagnosing the aortic arch disease is difficult because symptoms generally occur only after the artery has narrowed.
A physician will thoroughly review a patient's medical history to determine whether they suffer from another disease with similar symptoms and then perform a complete physical examination. In this examination, the doctor measures blood pressure and listens for abnormal whooshing sounds caused by blood rushing through a blood vessel through a stethoscope. After this, the procedure for aortic arch disease treatment cost in Hyderabad starts.
Physicians may also order the following tests:
-
Blood tests.
-
An artery is injected with contrast dye and x-rays are taken after it has been dyed.
-
Computed tomography (CT) scan.
-
Doppler ultrasound;
-
Magnetic resonance imaging (MRI).
-
Magnetic resonance angiography (MRA).
Treatment and Surgery
For the aortic arch disease, lifestyle modifications and medication are the first line of treatment. People with blood vessel inflammation and narrowing may be able to slow or prevent the progression of the disease by:
-
Quitting smoking
-
Exercising
-
Eating a diet low in saturated fat and cholesterol
-
Losing weight.
Aortic arch conditions are treated with the following medications:
-
Medications that lower blood pressure.
-
Medications to control the autoimmune response in Takayasu's arteritis.
An operation to widen or repair narrowed arteries may be required when aortic arch conditions become so advanced that arteries become blocked. It is common to perform an endarterectomy to remove plaque from the inner surface of arteries. Widening narrowed arteries can also be achieved with angioplasty, bypass surgery, and stenting.
Vertebral artery disease
The vertebral artery supplies blood to the brain. The disease known as vertebral artery disease can cause the brain to lose blood flow. A small piece (emboli) can also break off and block another artery leading to the brain or eye. A stroke occurs when the blood supply to the brain is disrupted - it is the third most common cause of death in the country.
Symptoms of vertebral artery disease
A transient ischemic attack (TIA) is one of the symptoms of a stroke. It may last a few minutes or up to 24 hours. The following symptoms require immediate attention:
-
Dizziness during exercise.
-
Double vision.
Risks of vertebral artery disease
Atherosclerosis increases the risk of getting the disease when fatty deposits or cholesterol build up in the blood vessels. People with peripheral artery disease are also more at risk. Other factors include:
-
Age and gender: Men are at higher risk before they reach 75, and women after they reach 75.
-
Diabetes.
-
Family history of this problem.
-
High blood pressure (hypertension).
-
High cholesterol.
-
Obesity.
-
Sedentary lifestyle.
-
Tobacco use: Smoking dramatically increases your risk.
Diagnosis
The most common tests for confirming vertebrobasilar disease are magnetic resonance angiography and standard angiography. Both utilize an injected dye to track the flow of blood and are useful for identifying stenosis or narrowing within blood vessels.
Treatment Options
A person with vertebrobasilar disease must change their lifestyle, including exercising, quitting smoking, eating a low-cholesterol diet, and controlling their diabetes. It may also be necessary to take medications that control cholesterol and platelet function, such as aspirin, Plavix, Lipitor, and Zocor. Additionally, depending on the specific cause and presentation of their condition, aortic arch syndrome treatment may be necessary to ensure adequate blood flow to the brain and upper body. CARE Hospitals also provide arrhythmia treatment in Hyderabad.
Surgical Options
- Endarterectomy: A surgical procedure to remove plaque from the affected arteries
- Bypass grafting
- Vertebral artery reconstruction
Endovascular Options
Angioplasty and stenting are procedures used to open narrowed coronary arteries using a catheter-guided balloon. Angioplasty usually involves placing a stent (a wire-mesh tube that expands to hold the artery open) at the narrowed section.
Carotid
The carotid arteries (which deliver blood to your brain and body) are clogged with fatty deposits (plaques). Blockages to the brain's blood supply increase your risk of stroke, which occurs when blood flow is interrupted or significantly reduced. Your brain is deprived of oxygen when you suffer a stroke. Within minutes, you begin to lose brain cells.
The development of coronary artery disease is slow. You may have a stroke or a transient ischemic attack (TIA) as the first sign that this condition exists. Temporary interruptions of the blood flow to your brain cause a TIA.
There are usually lifestyle changes, medications, and sometimes surgery involved in the treatment of carotid artery disease.
Causes
In the arteries that supply blood to the brain, plaques form and lead to coronary artery disease. There are microscopic injuries within arteries that cause plaques to form inside. A plaque is comprised of cholesterol, calcium, fibrous tissue, and other cellular debris. This process is known as atherosclerosis.
Plaques clogging the coronary arteries make them stiff and narrow. A clogged carotid artery makes it difficult for vital brain structures responsible for your daily functions to receive oxygen and nutrients.
Risk factors
The following factors increase your risk of carotid artery disease:
-
High blood pressure: The walls of arteries can be weakened by excessive pressure, making them susceptible to damage.
-
Tobacco use: It is known that nicotine can irritate your arteries. It is also known that smoking increases your blood pressure and heart rate.
-
Diabetes: Having diabetes affects your ability to process fat efficiently, putting you at greater risk of hypertension and atherosclerosis.
-
High blood-fat levels: The accumulation of plaques is promoted by high levels of low-density lipoprotein cholesterol and triglycerides, a type of blood fat.
-
Family history: Having a relative with atherosclerosis or coronary artery disease increases your risk of carotid artery disease.
-
Age: Our arteries lose flexibility as we age, thus increasing their vulnerability.
-
Obesity: Having a heavyweight increases your risk of heart disease, diabetes, and high blood pressure.
-
Sleep apnoea: Interruptions in breathing during sleep are associated with strokes.
-
Lack of exercise: High blood pressure, diabetes, and obesity can damage your arteries it.
Treatment
Treatment of carotid artery disease aims to prevent strokes. According to the extent of the blockage in your carotid arteries, you may need specific treatments.
Depending on the severity of the blockage, your doctor may recommend:
-
Changing your lifestyle to slow the progression of atherosclerosis: There may be recommendations to quit smoking, lose weight, eat healthy foods, reduce salt, and exercise regularly.
-
Medication to lower blood pressure or cholesterol may be prescribed: To prevent blood clots, your doctor may also recommend that you take daily aspirin.
A doctor may recommend removing the blockage from the artery if the blockage is severe, or if you have already had a TIA or stroke. Among the options are:
-
Carotid endarterectomy is the most common treatment for severe carotid artery disease. In a surgical procedure, a surgeon makes an incision along the front of your neck and opens up the carotid artery to remove plaque. After the artery has been repaired, it is stitched or grafted.
-
The carotid artery can be stented and angioplasty if you have a blockage that is too difficult to reach with a carotid endarterectomy or if you suffer from other health conditions that make surgery too risky. During treatment, you will be given local anaesthesia, and a tiny balloon will be threaded into the clog using a catheter. The balloon expands the artery, and a wire mesh coil (stent) maintains its widening.
Diagnosis
During your first visit, your doctor will probably conduct a thorough medical history and physical examination. Generally, the exam entails listening for a swooshing sound (bruit) over the carotid artery in your neck, which is indicative of a narrowed artery. A doctor may then perform physical and mental tests on you, such as strength, memory, and speech.
Following that, your doctor may recommend:
-
An ultrasound is used to assess blood flow and pressure in the carotid arteries.
-
CT or MRI can detect strokes or other abnormalities.
-
MR angiography or CT angiography, which provides additional pictures of blood flow in the carotid arteries. CT scans and MRIs gather images of your neck and brain after injecting contrast dye into blood vessels.
Our Doctors
-

Dr. Tarun Gandhi
MS, FVES
Vascular & Endovascular Surgery
View More -

Dr. P C Gupta
MBBS, MS, FICA, FIVS (Japan)
Vascular & Endovascular Surgery
View More -

Dr. Ashish N Badkhal
MBBS, MS, MCh
Vascular Surgery
View More -

Dr. Ashok Reddy Somu
MBBS, MD, FVIR
Vascular & Interventional Radiology
View More -

Dr. B. Pradeep
MBBS, MD, DNB, FRCR CCT (UK)
Vascular & Interventional Radiology
View More -

Dr. Mustafa Razi
MBBS, MD
Vascular & Interventional Radiology
View More -

Dr. N. Madhavilatha
MBBS, MS, PDCC
Vascular & Endovascular Surgery
View More -

Dr. Radhika Malireddy
MBBS, DNB (General Surgery), DrNB (Plastic & Reconstructive Surgery), Post-Doctoral Fellowship in Diabetic Foot Surgery
Vascular & Endovascular Surgery
View More -

Dr. Rahul Agarwal
MBBS, DNB (General Surgery), FMAS, DrNB (Vasc. Surg)
Vascular & Endovascular Surgery
View More -

Dr. Rajesh Poosarla
MBBS, MD, DNB, DM (Gold Medalist), EBIR, FIBI, MBA (HA)
Interventional Radiology
View More -

Dr. S. Chainulu
MBBS, DNB (Radio-Diagnosis)
Vascular & Interventional Radiology
View More -

Dr. Sadath Ahmed
MBBS, DrNB (CTVS)
Cardiac Surgery, Vascular Surgery
View More -

Dr. Sailaja Vasireddy
MBBS, DrNB (CTVS)
Cardiac Surgery, Vascular Surgery
View More -

Dr. Santhosh Reddy K
MBBS, MD
Radiology
View More -
Dr. Sudheer Gandrakota
MBBS, DNB, CTVS
Cardiac Surgery, Vascular Surgery
View More -

Dr. Surya Kiran Indukuri
MBBS, MS (General Surgery), DrNB (Vascular & Endovascular Surgery)
Vascular & Endovascular Surgery
View More -

Dr. V. Apoorva
MBBS, MS (General Surgery), DrNB Vascular surgery
Vascular & Endovascular Surgery
View More -

Dr. Vamsi Krishna Yerramsetty
MBBS, DNB, FIVS
Vascular & Endovascular Surgery
View More -

Dr. Venugopal Kulkarni
MBBS, MS, MRCS, FRCS
Vascular & Endovascular Surgery
View More -

Dr. Vivek Lanje
MBBS, DNB (General Surgery), Mch (Cardiovascular & Thoracic Surgery)
Vascular Surgery
View More
Frequently Asked Questions
Couldn’t find what you were looking for?
Need any help? Get a Call Back.

Still Have a Question?

