-
Doctors
-
Specialities & Treatments
Centre of Excellence
Specialties
Treatments and Procedures
Hospitals & Directions HyderabadCARE Hospitals, Banjara Hills CARE Outpatient Centre, Banjara Hills CARE Hospitals, HITEC City CARE Hospitals, Nampally Gurunanak CARE Hospitals, Musheerabad CARE Hospitals Outpatient Centre, HITEC City CARE Hospitals, Malakpet
HyderabadCARE Hospitals, Banjara Hills CARE Outpatient Centre, Banjara Hills CARE Hospitals, HITEC City CARE Hospitals, Nampally Gurunanak CARE Hospitals, Musheerabad CARE Hospitals Outpatient Centre, HITEC City CARE Hospitals, Malakpet Raipur
Raipur
 Bhubaneswar
Bhubaneswar Visakhapatnam
Visakhapatnam
 Nagpur
Nagpur
 Indore
Indore
 Chh. Sambhajinagar
Chh. SambhajinagarClinics & Medical Centers
Book an AppointmentContact Us
Online Lab Reports
Book an Appointment
Consult Super-Specialist Doctors at CARE Hospitals

Patellar Tendinopathy
Symptom, Causes, Diagnosis and Treatment
Patellar Tendinopathy
Patellar tendinopathy affects many elite jumping athletes during their careers. Young athletes between 15-30 years old, particularly men who play sports with repetitive jumps, commonly develop this painful knee condition, also known as jumper's knee.
Elite basketball and volleyball players have the highest risk. Athletes in football, tennis, and jump events frequently experience this tendon problem too. The knee's patellar tendon weakens from repeated movements, leading to patellar tendinopathy. Recovery options are available effectively. Physical therapy that strengthens the quadriceps muscles serves as the foundation for most patients' recovery. Athletes can return to their activities successfully with accurate diagnosis and customised rehabilitation, despite this condition's prevalence.\
What is Patellar Tendinopathy?
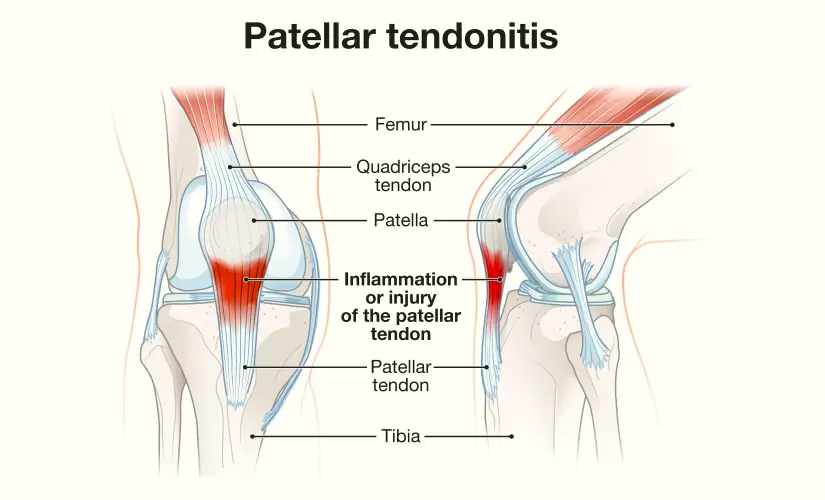
Your patellar tendon links your kneecap (patella) to your shin bone (tibia) and works with the quadriceps muscle to move your knee. Small tears develop in this tendon from overuse, and these tears weaken it gradually. Athletes who jump frequently get this condition so often that people call it "jumper's knee." Doctors originally called it patellar tendinitis. Research shows this condition lacks traditional inflammatory cells, which makes it a degenerative condition rather than an inflammatory one.
Patellar Tendinopathy Symptoms
People with this condition feel a dull ache at the front of their knee, usually just below the kneecap. The pain gets worse during activities that put pressure on the tendon, especially when jumping, running, or climbing stairs. The pain tends to go away almost right after stopping these activities. Common symptoms include:
- Pain and tenderness below the kneecap
- Stiffness, usually in the morning
- Problems bending or straightening the knee
- Pain that gets worse with physical activity
In severe cases, people might experience constant pain that stops their performance.
Causes of Patellar Tendinopathy
The patellar tendon develops tiny tears when it faces repeated stress without enough time to heal. These tears don't heal properly when people keep overloading the tendon. Some movements put extra strain on the tendon:
- Jumping and landing repeatedly
- Quick increases in training intensity
- Sprinting and rapid direction changes
- Training on hard surfaces
Studies show that an athlete's landing technique might affect their risk. Athletes who land more stiffly have higher rates of tendinopathy.
Risk Factors
Several things can make you more likely to get this condition. Men get patellar tendinopathy twice as often as women. This might happen because male tendons face stronger forces from stronger quadriceps muscles. Other risk factors include (but are not limited to):
- People between 15-30 years old
- Jumping on hard surfaces like concrete
- Higher body weight or BMI
- Unbalanced muscles
- Tight quadriceps or hamstrings
- Physical differences like uneven leg lengths
Complications
This condition can become long-lasting and severe without proper treatment. Many volleyball players with jumper's knee end up leaving competitive play because their symptoms won't go away. The condition can lead to reduced knee function that lasts for years after the original diagnosis. Daily activities become harder with chronic pain, and in rare cases, the patellar tendon can tear completely, requiring surgery.
Diagnosis of Patellar Tendinopathy
Doctors diagnose jumper's knee through a detailed clinical examination. They check for tenderness just below the kneecap and assess how pain changes with knee movement. Pain at the inferior pole of the patella and discomfort that increases during knee extension activities are the key signs.
Basset's sign helps doctors confirm the diagnosis. This test checks tenderness during knee extension and flexion. A positive result shows reduced pain when the knee flexes.
Imaging tests can provide extra confirmation, though they aren't always needed:
- X-rays help rule out other bone problems
- Ultrasound reveals tendon thickening and abnormalities
- MRI shows detailed changes in chronic cases
Patellar Tendinopathy Treatment
Doctors prefer conservative methods over immediate surgery as the first treatment option:
- Rest and Modification: Cut back on tendon-loading activities without stopping completely.
- Physical Therapy: Eccentric exercises are the foundation of rehabilitation. Decline squats have shown good results for both athletes & non-athletes. Heavy, slow resistance exercises also show promising outcomes.
- Pain Management: Ice, elevation, and over-the-counter medications help manage discomfort.
- These additional options exist for severe cases:
- Platelet-rich plasma injections
- Extracorporeal shock wave therapy
- Surgical intervention: Doctors typically suggest surgery after 3-6 months of unsuccessful conservative treatment. Your surgeon removes damaged patellar tissue either through open surgery or arthroscopy.
Low-Dose Radiation Therapy (LDRT) for Patellar Tendinopathy
Low-Dose Radiation Therapy is an emerging, noninvasive treatment that can help to decrease the long-lasting pain. It reduces inflammatory activity and improves blood flow in the affected tendon region. Your doctor may consider LDRT for chronic patellar tendinopathy, as it gives pain relief and functional improvement without the surgery. The therapy is administered over a few short sessions and is generally well-tolerated with minimal side effects.
When to See a Doctor
Contact your doctor if:
- Your knee pain lasts more than a few days despite home treatment
- You notice swelling or can't bear weight
- You can't fully bend or extend your knee
- Your symptoms get worse
- Your knee feels warm to the touch; that indicates possible inflammation
- Pain that affects your exercise routine or daily activities needs professional evaluation.
Prevention
Your knees need a comprehensive approach to stay protected from patellar tendinopathy. Sports medicine experts agree that your body needs adequate recovery time between intense activities. Rest days will give your tendons time to repair and adapt to physical demands.
- Proper warm-up gets your body ready for exercise. A 5-10 minute walk or dynamic stretches boost blood flow to muscles and tendons. This makes them more flexible and reduces injury risk. You should cool down & stretch your body after physical activity.
- Strengthening exercises for leg muscles give better support to your knees. Eccentric exercises have proven benefits as muscles lengthen while returning to their starting position. Wall squats, straight leg raises, and step-ups build strength in the quadriceps, hamstrings, and calf muscles. These exercises help distribute force better across the knee joint.
- Strength and flexibility go hand in hand. Regular stretching of thigh muscles, hamstrings, and calves helps in the following (including but not limited to):
- Reduce muscle spasms
- Decrease pressure on tendons
- Improve range of motion
Bad technique puts extra stress on knee joints. A coach or trainer can help you maintain correct form during sports and exercises to lower your injury risk. Cross-friction massage and ice massage break down scar tissue and reduce inflammation.
The biggest mistake is trying to "play through the pain" when your knees hurt. This can turn a minor problem into a chronic condition. Listen to your body's signals and modify activities when needed.
Athletes returning to sports or starting new workouts should increase intensity gradually. Unprepared tendons struggle with sudden increases in training volume.
People with flat feet might benefit from orthotics (an insert that fixes biomechanical problems causing extra stress on the patellar tendon).
Conclusion
Patellar tendinopathy creates real challenges if you have an active lifestyle, especially when you play jumping sports. This condition affects many athletes, but spotting symptoms early helps speed up recovery. Watch out for pain below the kneecap—it's a warning sign you shouldn't ignore.
Note that pushing through knee pain usually makes things worse. Your best move is to adjust your training routine as soon as you feel discomfort. Recovery might take time. A smart approach to treatment and prevention helps most people return to their favorite activities with healthy knees that last.
FAQs
1. How common is patellar tendinopathy?
Patellar tendinopathy affects different groups of people at varying rates. The general population sees very low rates. Athletes tell a different story. Many athletes deal with this condition, including volleyball, basketball and soccer players topping the list. Age makes a difference too. Athletes over 18 are more likely to get it. Men face this condition more often than women.
2. How do you treat patellar tendinopathy?
Treatment usually starts with basic approaches:
- Rest and activity modification - Cut back on activities that make it worse
- Exercise therapy - Seven out of ten patients see great results with eccentric exercises
- Heavy, slow resistance training - Patients improve both quickly and over time
- Isometric exercises - These help reduce pain right away
Severe cases might need:
- Platelet-rich plasma injections
- Extracorporeal shockwave therapy
- Cryotherapy (10-minute treatments through wet towels work best)
Doctors consider surgery only after other treatments haven't worked for 6 months.
3. Does patellar tendinopathy go away?
Patellar tendinopathy usually heals with the right treatment. Mild cases can clear up in six weeks. Severe cases might take 3-6 months to heal fully. Some people need more time.
Recovery isn't guaranteed. One-third of patients can't get back to sports within six months. The numbers look worse for elite athletes—half of them end up retiring from their sport. Your chances of recovery get better when you stick to a well-laid-out rehab programme. Most soft tissue injuries heal well with proper care.
4. Is walking good for patellar tendinopathy?
Walking is usually safe when you have patellar tendinopathy. Moving around helps blood flow, keeps joints mobile, and boosts overall health. Staying completely still might actually make things worse. Your body will tell you when to stop if the pain increases. Athletes getting back to their routine should try these walking tips:
- Warm up your quadriceps first
- Keep your posture straight
- Stay off hills that stress your knees
- Slow down if you feel pain
High-impact activities should wait until your knee heals, even though walking is usually safe for the healing tendon.

Still Have a Question?

