-
Doctors
-
Specialities & Treatments
Centre of Excellence
Specialties
Treatments and Procedures
Hospitals & Directions HyderabadCARE Hospitals, Banjara Hills CARE Outpatient Centre, Banjara Hills CARE Hospitals, HITEC City CARE Hospitals, Nampally Gurunanak CARE Hospitals, Musheerabad CARE Hospitals Outpatient Centre, HITEC City CARE Hospitals, Malakpet
HyderabadCARE Hospitals, Banjara Hills CARE Outpatient Centre, Banjara Hills CARE Hospitals, HITEC City CARE Hospitals, Nampally Gurunanak CARE Hospitals, Musheerabad CARE Hospitals Outpatient Centre, HITEC City CARE Hospitals, Malakpet Raipur
Raipur
 Bhubaneswar
Bhubaneswar Visakhapatnam
Visakhapatnam
 Nagpur
Nagpur
 Indore
Indore
 Chh. Sambhajinagar
Chh. SambhajinagarClinics & Medical Centers
Book an AppointmentContact Us
Online Lab Reports
Book an Appointment
Consult Super-Specialist Doctors at CARE Hospitals

Pulmonary Embolism
Symptom, Causes, Diagnosis and Treatment
Pulmonary Embolism
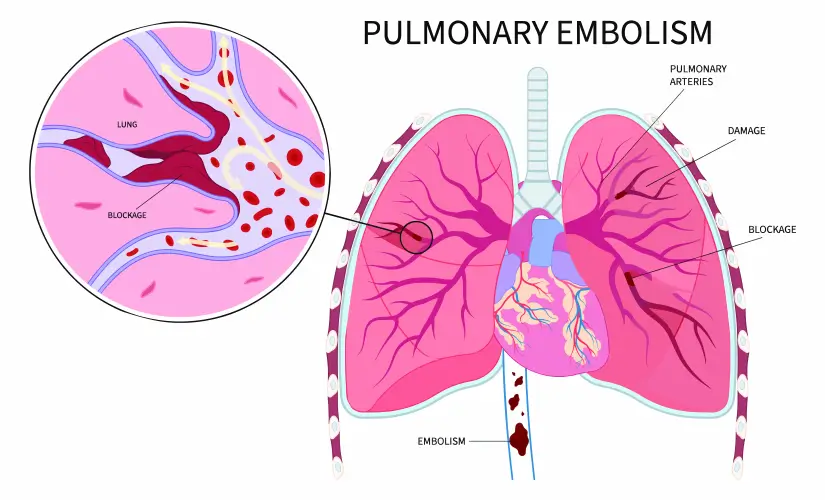
A blood clot that gets embroiled in your lung artery can cause a pulmonary embolism by blocking crucial blood flow. The survival rate is concerning - one in three people who don't get diagnosed and treated don't make it. The good news is that rapid identification and treatment significantly improve these odds.
Most patients experience sudden shortness of breath as their primary symptom, though other signs can differ from person to person. Blood thinners, or anticoagulants, serve as the primary treatment option. Your chances of survival increase dramatically if you know the risk factors, spot the symptoms early, and get medical help right away.
What is Pulmonary Embolism?
The condition occurs when blood clots break free from deep leg veins (deep vein thrombosis or DVT) and lodge themselves in smaller lung arteries. Blood vessel blockages can sometimes result from air bubbles, fat, amniotic fluid, or tumour cells, though these cases are rare.
Symptoms of Pulmonary Embolism
The clot's size and affected lung area determine how pulmonary embolism symptoms present themselves. People commonly experience:
- Sudden breathing difficulties (most common symptom)
- Severe chest pain that gets worse while breathing
- Coughing episodes, sometimes with blood
- Fast breathing and elevated heart rate
Some patients might feel dizzy, anxious, or faint. They could also experience heavy sweating and notice their lips or nails turning bluish.
Causes of Pulmonary Embolism
Surgery, trauma, infections, or injuries can damage veins and lead to blood clots. Blood tends to pool and form clots during long periods without movement.
Risks of Pulmonary Embolism
People face higher PE risks if they:
- Have passed age 60
- Recently underwent surgery, particularly joint replacements.
- Live with cancer or receive chemotherapy
- Experience pregnancy or recent childbirth
- Take hormone-based medicines
- Have relatives with a blood clot history
- Stay immobile during extended travel
Complications of Pulmonary Embolism
Delayed treatment can result in:
- High blood pressure in lung vessels (pulmonary hypertension)
- Right-sided heart failure from excessive strain
- Dead lung tissue (pulmonary infarction)
- Fluid collecting around lungs (pleural effusion)
Diagnosis
A doctor's first steps include a physical examination and a review of your medical history. They check your legs to find signs of deep vein thrombosis—looking for swollen, tender, red, or warm areas.
Blood tests that measure D-dimer levels help detect clot formation, and high levels might point to blood clots.
Several imaging tests may be needed:
- CT pulmonary angiography (the most common method)
- Ultrasound of legs to detect clots
- Ventilation-perfusion (V/Q) scan
- Echocardiogram to assess heart function
- Pulmonary angiography to confirm diagnosis in unclear cases
Treatments for Pulmonary Embolism
The main goal of pulmonary embolism treatment is to stop the growth of clots and prevent new ones from forming.
Blood thinners (anticoagulants) are the standard treatment option. These medications let your body break down existing clots naturally instead of dissolving them directly.
Doctors might use thrombolytics (clot dissolvers) in life-threatening cases, though these carry a higher bleeding risk.
Severe cases might need surgical intervention through catheter-assisted clot extraction or placement of a vena cava filter that stops clots from reaching the lungs.
When to See a Doctor
You need immediate medical care if you experience unexplained breathing difficulty, chest pain, or fainting.
Patients taking blood thinners should contact their doctor if they notice black stools, severe headaches, or growing bruises—these could signal internal bleeding.
Prevention
You can take several steps to prevent pulmonary embolism:
- Moving regularly, especially during long trips
- Wearing compression stockings to improve blood flow
- Staying hydrated and limiting alcohol intake
- Staying away from tobacco
- Keeping a healthy weight
- Raising your legs for 30 minutes twice each day
Surgical patients often receive blood thinners before and after procedures to lower their risk of developing clots.
Conclusion
Pulmonary embolism is a serious medical condition. You and your doctor can manage it if detected early. Understanding this condition can help patients and their families take the right steps, even though the original diagnosis might be scary. Your body will send warning signals through sudden breathing problems or chest pain. A quick response to these symptoms can save your life.
Risk factors affect people in different ways based on their age, medical history, and lifestyle choices. Long periods without movement increase the risk, especially after surgery or during extended travel. Your risk also goes up with pregnancy, hormone medications, and family history - these all play important roles.
Most people can benefit from prevention strategies. The advanced imaging technologies, combined with treatments like anticoagulants, give hope to patients with severe cases. Medical advances improve outcomes each year. Quick intervention gives patients the best chance of survival and many return to healthy lives after treatment.
Note that breathlessness, chest pain, or unusual symptoms need immediate medical care. Taking action today stops complications tomorrow.
FAQs
1. What is the main cause of a pulmonary embolism?
Blood clots developing in deep leg veins (deep vein thrombosis or DVT) cause all but one of these pulmonary embolisms. Blood pools in your veins during inactive periods, especially after surgery or long trips. Other substances can block blood flow in rare cases:
- Fat released after bone fractures or trauma
- Air bubbles from surgery or medical procedures
- Tumour cells from fast-growing cancers
- Amniotic fluid
2. Can you recover from a pulmonary embolism?
The right treatment helps most people recover completely. Recovery takes several weeks or months as symptoms get better with ongoing treatment. Some patients feel better once treatment starts, though breathing problems or chest pain might last for weeks. Quick treatment saves lives.
3. What are the warning signs of a pulmonary embolism?
The following are common warning signs:
- Sudden shortness of breath (most common symptom)
- Sharp chest pain gets worse with breathing or coughing
- Fast heartbeat or irregular pulse
- Coughing up blood
- Anxiety, lightheadedness, or fainting
- Bluish lips or nails in severe cases
4. Can pulmonary embolism be cured?
Blood-thinning medications help your body dissolve the clot over time, though "cure" isn't the best word. Most patients need anticoagulants for at least three months, sometimes longer. Lifelong medication might help people with a higher risk of recurrence. The condition rarely comes back if you follow proper treatment and prevention steps.
5. Can an ECG detect pulmonary embolism?
Doctors cannot diagnose pulmonary embolism with an ECG alone. ECG changes show up in many PE cases, but they're not specific or sensitive enough for diagnosis. All the same, ECGs help rule out other problems like heart attacks. CT pulmonary angiography, D-dimer blood tests, and lung scans give more reliable results.
6. Does PE permanently damage lugs?
Most patients don't get serious permanent lung damage. A small group develops scar tissue in lung arteries that leads to chronic thromboembolic pulmonary hypertension (CTEPH). This scarring affects breathing. You should ask your doctor about this rare complication if you still have trouble breathing six months after treatment.
To Book an Appointment, call:
Still Have a Question?


