-
Doctors
-
Specialities & Treatments
Centre of Excellence
Specialties
Treatments and Procedures
Hospitals & Directions HyderabadCARE Hospitals, Banjara Hills CARE Outpatient Centre, Banjara Hills CARE Hospitals, HITEC City CARE Hospitals, Nampally Gurunanak CARE Hospitals, Musheerabad CARE Hospitals Outpatient Centre, HITEC City CARE Hospitals, Malakpet
HyderabadCARE Hospitals, Banjara Hills CARE Outpatient Centre, Banjara Hills CARE Hospitals, HITEC City CARE Hospitals, Nampally Gurunanak CARE Hospitals, Musheerabad CARE Hospitals Outpatient Centre, HITEC City CARE Hospitals, Malakpet Raipur
Raipur
 Bhubaneswar
Bhubaneswar Visakhapatnam
Visakhapatnam
 Nagpur
Nagpur
 Indore
Indore
 Chh. Sambhajinagar
Chh. SambhajinagarClinics & Medical Centers
Book an AppointmentContact Us
Online Lab Reports
Book an Appointment
Consult Super-Specialist Doctors at CARE Hospitals

Spondylolisthesis
Symptom, Causes, Diagnosis and Treatment
Spondylolisthesis
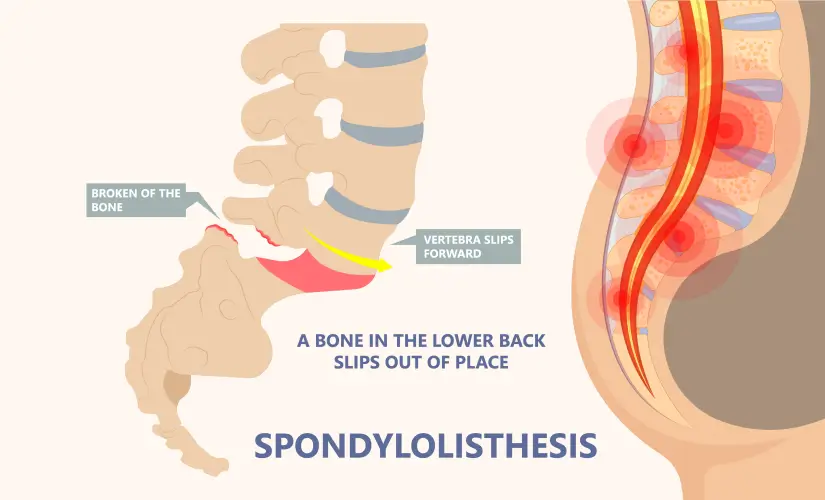
Spondylolisthesis is a spine-related condition that develops when a vertebra slides forward over the one beneath it. While most cases occur in the lower back, some patients experience it in their neck or mid-back region.
This article covers everything about spondylolisthesis—from its types and symptoms to causes and treatments. Readers will also learn the right time to consult a doctor and ways to handle this condition.
What is Spondylolisthesis?
Spondylolisthesis comes from Greek words meaning "vertebra" and "to slip." This condition arises when one vertebra slips forward (anterolisthesis) or backward (retrolisthesis) over the next vertebra. Spondylolisthesis usually develops in the lower back (lumbar spine), especially at the L5-S1 level, though it can sometimes affect the cervical spine.
Types of Spondylolisthesis
Doctors group spondylolisthesis into six main types based on what causes them:
- Degenerative Spondylolisthesis: Adults over 50 commonly get this type from normal wear and tear of discs and joints
- Isthmic Spondylolisthesis: A stress fracture in the pars interarticularis causes this, and it's common in young athletes
- Dysplastic/Congenital Spondylolisthesis: People are born with this due to vertebrae that didn't form right
- Traumatic Spondylolisthesis: This happens after serious injuries from accidents or falls
- Pathologic Spondylolisthesis: Diseases like tumours, infections, or osteoporosis lead to this type
- Iatrogenic Spondylolisthesis: This shows up after complications from spine surgery
Symptoms of Spondylolisthesis
Some people with spondylolisthesis don't feel any symptoms. But those who do might experience the following spondylolisthesis symptoms:
- Back pain that gets worse while standing or walking
- Pain that spreads to buttocks and thighs
- Tight hamstring muscles
- Legs feeling numb, tingly or weak
- Problems bending forward
- Back stiffness
Spondylolisthesis Causes
Several things can make vertebrae slip. The spine naturally weakens with age, and repeated activities that stretch the spine too far can create stress fractures. Genes play a part since this condition sometimes runs in families. Athletes who do gymnastics, football, weightlifting, and track put a lot of strain on their lower backs, which increases their risk. People born with spine alignment problems might also be more likely to get this condition.
Risks of Spondylolisthesis
Some people have a higher chance of getting spondylolisthesis.
- Women get degenerative spondylolisthesis about three times more often than men.
- Black women's risk is three times higher than white women's.
- More than the optimal body weight puts more pressure on the spine.
- Young people who do activities that stretch their lower spine too much face a higher risk.
Complications of Spondylolisthesis
Spondylolisthesis can cause serious problems if left untreated.
- Nerve roots often get pinched where the slippage occurs.
- Spinal stenosis (a narrow spinal canal)
- Cauda equina syndrome (affecting how you control your bladder/bowels)
- Long-term back pain
Diagnosis
Doctors use physical examinations and imaging tests to diagnose spondylolisthesis. The examination usually involves patients lying down to raise one leg straight up. This movement often causes pain in patients who have tight hamstrings or sciatica from spondylolisthesis. X-rays serve as the starting point to show if a vertebra has moved forward.
Doctors might need additional tests to get a complete picture:
- MRI scans - best option to evaluate soft tissues and nerve compression
- CT scans - show detailed bone structure and fractures clearly
- Bone scans - help track active fracture healing
Treatments for Spondylolisthesis
- Noninvasive treatment: Non-surgical spondylolisthesis treatment works well for most patients. The standard approach starts with:
- Rest and changing activity levels
- Anti-inflammatory medications such as ibuprofen
- Physical therapy that builds core strength and stretches hamstrings
- Epidural steroid injections to reduce pain
- Bracing that keeps the spine stable
- Spondylolisthesis surgery: Surgical options come into play if conservative treatments don't work after 3-6 months or neurological symptoms get worse. These procedures include spinal decompression (laminectomy) to free trapped nerves and spinal fusion to stabilise affected vertebrae.
When to See a Doctor
Back pain that lasts more than 3-4 weeks needs medical attention, especially if the pain spreads to your thighs or buttocks. Don't wait to get emergency care if you experience groin numbness, lose bladder or bowel control, or have trouble walking. These symptoms might point to cauda equina syndrome, a serious condition that needs immediate treatment.
Prevention
You can't completely prevent spondylolisthesis, but these strategies help reduce your risk:
- Keep your weight in check to ease spine pressure
- Build strong core muscles through regular exercise
- Use good posture throughout the day
- Pick low-impact activities like swimming or cycling
- Get enough calcium and vitamin D to keep bones healthy
Spondylolisthesis vs Spondylosis
| Condition | Description |
| Spondylosis | Degenerative changes in the spine related to ageing, including disc degeneration and osteophyte formation |
| Spondylolysis | A specific defect or stress fracture in the pars interarticularis of a vertebra, often leading to spondylolisthesis |
Conclusion
Spondylolisthesis is a common spinal condition that many adults worldwide can manage well. The name might sound complex, but understanding and treating this condition can be simple. Most patients with Grade I spondylolisthesis (the most common type) can lead normal, active lives with proper care. Conservative treatments help many people effectively, and surgery can provide relief when symptoms become severe.
Quick diagnosis is vital to prevent complications like chronic pain or nerve damage. Persistent back pain, especially with leg symptoms, should prompt a medical visit before the condition worsens. Patients need to follow their doctor's guidance and never miss follow-up appointments.
FAQs
1. What foods are good for spondylolisthesis?
A healthy diet is vital in managing spondylolisthesis. The right foods can reduce inflammation & support bone health.
Foods with high omega-3 fatty acids help decrease inflammation in the body. Salmon, mackerel, walnuts, and flaxseeds are great choices.
Dark leafy greens also boost recovery after spinal injuries.
- Calcium-rich foods (dairy products, leafy greens)
- Vitamin D sources (fatty fish, egg yolks)
- Magnesium-rich foods (spinach, nuts, whole grains)
- Turmeric (contains anti-inflammatory curcumin)
- Berries (contain antioxidants that remove toxins)
2. Can spondylolisthesis be cured without surgery?
Most people respond well to non-surgical treatments. Surgery becomes necessary only in severe cases. Treatment options include:
- Rest and activity modification
- Anti-inflammatory medications
- Physical therapy to strengthen core muscles
- Epidural steroid injections
- Bracing to stabilise the spine
3. Is walking good for spondylolysis?
Walking is an excellent, low-impact activity if you have spondylolysis. Light exercise increases blood flow to your spine and speeds up recovery. High-impact activities can make symptoms worse, so avoid them until pain subsides.
4. How did I cure my spondylitis naturally?
People manage spondylitis symptoms through lifestyle changes. Regular stretching builds flexibility and reduces pain. Warm baths or heating pads help decrease stiffness before exercise. Ice packs work well to reduce inflammation after activity.
5. How long is the recovery time for spondylolisthesis?
Recovery from spondylolisthesis takes 6 to 12 weeks. Your healing time depends on your health, how severe the slippage is, and what treatment you choose. Surgical patients might need up to a year to recover completely.
6. Is spondylolisthesis serious?
Spondylolisthesis can range from mild to severe. Without treatment, it leads to chronic back pain, spinal stenosis, and nerve damage. Severe cases can cause permanent nerve damage with leg weakness and paralysis.
7. What food should be avoided in spondylitis?
Foods that cause inflammation can make your back pain worse. Stay away from:
- Sugary foods (sodas, candies, sweetened cereals)
- High-fat foods (red meat, French fries)
- Dairy products, especially processed cheeses
- Refined grains (white bread, pasta)
- Processed foods with additives and preservatives
Still Have a Question?


