-
Doctors
-
Specialities & Treatments
Centre of Excellence
Specialties
Treatments and Procedures
Hospitals & Directions HyderabadCARE Hospitals, Banjara Hills CARE Outpatient Centre, Banjara Hills CARE Hospitals, HITEC City CARE Hospitals, Nampally Gurunanak CARE Hospitals, Musheerabad CARE Hospitals Outpatient Centre, HITEC City CARE Hospitals, Malakpet
HyderabadCARE Hospitals, Banjara Hills CARE Outpatient Centre, Banjara Hills CARE Hospitals, HITEC City CARE Hospitals, Nampally Gurunanak CARE Hospitals, Musheerabad CARE Hospitals Outpatient Centre, HITEC City CARE Hospitals, Malakpet Raipur
Raipur
 Bhubaneswar
Bhubaneswar Visakhapatnam
Visakhapatnam
 Nagpur
Nagpur
 Indore
Indore
 Chh. Sambhajinagar
Chh. SambhajinagarClinics & Medical Centers
Book an AppointmentContact Us
Online Lab Reports
Book an Appointment
Consult Super-Specialist Doctors at CARE Hospitals
Rotablation Angioplasty: Benefits, Treatments, And Recovery Time
Updated on 9 May 2025
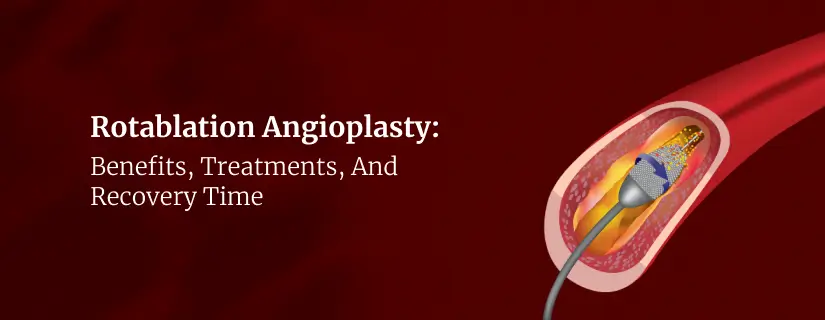
Rotablation Angioplasty is effective for patients with heavily calcified arterial blockages that traditional balloon angioplasty cannot address effectively. As a minimally invasive treatment option, it offers quicker recovery times compared to open-heart surgery, making it especially beneficial for elderly patients with complex coronary artery disease.
This guide explores the essential aspects of rotablation angioplasty, including its benefits, treatment process, and what patients can expect during the procedure.
What is Rotablation Angioplasty?
Rotablation angioplasty is a specialised technique for treating complex arterial blockages that conventional angioplasty methods cannot effectively address. Unlike traditional angioplasty, which presses the plaque against artery walls with a balloon, rotablation uses rotational forces to break down and physically remove hard, calcified deposits. This distinction makes rotablation exceptionally valuable when dealing with severely calcified lesions or extremely narrow passages where standard balloon catheters cannot pass through.
The cornerstone of rotablation technology is a flexible catheter with a small diamond-coated burr at its tip. When activated, this burr spins at remarkably high speeds—between 140,000 and 180,000 rotations per minute—effectively drilling through the hardened plaque that blocks the artery. The diamond-coated surface works like a microscopic grinding tool, pulverising the calcified deposits into tiny particles.
Benefits of Rotablation Angioplasty
The unique advantages of rotablation angioplasty make it a superior choice for patients with complex coronary artery disease. This procedure offers remarkable benefits compared to conventional treatment approaches for those with heavily calcified arterial blockages.
The diamond-coated burr selectively targets and breaks down calcified plaque while preserving the structural integrity of the vessel wall. This precision mechanism enables interventional cardiologists to treat complex lesions that might not respond well to standard angioplasty techniques alone.
The procedure creates an optimal environment for stent expansion and proper positioning against the arterial wall by thoroughly grinding away calcified deposits. This meticulous preparation reduces the risk of stent malapposition—a condition associated with serious complications like stent thrombosis and restenosis.
For patients with severe blockages, rotablation angioplasty provides several crucial benefits:
- Opens severely blocked arteries, particularly those resistant to conventional balloon angioplasty
- Improves blood circulation to the heart, reducing chest pain and heart attack risk
- Offers a minimally invasive alternative with quicker recovery compared to bypass surgery
- Reduces procedural complications such as vessel dissection and perforation
- Preserves the structural integrity of treated blood vessels
- Patients who might not qualify for other revascularisation procedures can benefit from rotablation angioplasty.
Most patients can return home the same day or within 24 hours after the procedure. This rapid recovery stands in stark contrast to traditional open-heart surgeries, which require lengthy hospital stays and extended recuperation periods.
Purpose of Rotablation Angioplasty Procedure
The primary objective of rotablation is plaque modification through debulking. By removing hardened calcified material, the rotablation procedure improves vessel compliance, preparing arteries for subsequent balloon expansion and stent placement. This preparation is crucial for optimal stent deployment, allowing for better apposition against vessel walls and reducing long-term complications.
Several specific clinical scenarios call for rotablation angioplasty:
- Heavily calcified coronary lesions that balloons cannot penetrate or dilate
- Diffusely diseased vessels requiring modification before balloon treatment
- Aorto-ostial lesions (blockages at the junction where coronary arteries connect to the aorta)
- Angulated stenoses that present challenging access for conventional devices
- In-stent restenosis (re-narrowing within previously placed stents)
- Extremely narrow passages where standard balloons cannot pass through
- High-risk elderly patients with complex coronary disease.
Treatment Process of Rotablation Angioplasty
Performing rotablation angioplasty requires specialised equipment and expert precision. Skilled interventional cardiologists typically carry it out in a dedicated cardiac catheterisation laboratory.
The rotablation process involves several key steps:
- A guide wire is carefully threaded through the artery until it reaches the blockage
- A special catheter with a diamond-coated burr at its tip is inserted along the wire
- Once in position, the burr spins at exceptionally high speeds, powered by compressed air
- The rotating burr gradually chips away at the hard, calcified plaque to widen the narrowing
- Microscopic plaque particles created during drilling are naturally washed away in the bloodstream
- After successfully breaking down the calcium deposits, the surgeon inserts a balloon
- The procedure continues as a standard angioplasty with balloon dilation and stent placement
Following rotablation angioplasty, patients remain under close observation for several hours. Medical staff vigilantly monitor vital signs and blood flow patterns to detect any potential complications early. Most individuals can return home either the same day or within 24 hours, though this timeline may vary based on individual circumstances.
Post-procedure care involves several essential elements. Doctors commonly prescribe antiplatelet and anticoagulant medications to prevent blood clots and support healing.
Ongoing check-ups and follow-up appointments play a crucial role in monitoring recovery progress. These visits allow doctors to assess the effectiveness of the procedure, make necessary treatment adjustments, and offer continued guidance on maintaining optimal cardiovascular health over time.
Difference Between Traditional and Rotablation Angioplasty
Both techniques aim to improve blood flow through narrowed coronary arteries, yet they employ distinctly different approaches to tackle arterial blockages.
| Feature | Traditional Angioplasty | Rotablation Angioplasty |
| Basic Technique | Uses a balloon to press plaque against artery walls | Employs a diamond-coated burr that drills through calcified plaque |
| Mechanism of Action | Compresses plaque without removing it | Physically breaks down and removes hardened plaque deposits |
| Ideal For | Softer, non-calcified blockages | Heavily calcified or fibrous plaques that resist balloon dilation |
| Equipment Used | Guidewire and balloon catheter | Guidewire, a special catheter with a drill tip powered by compressed air |
| Stent Requirement | Higher stent requirement | Lower stent requirement |
| Effectiveness for Complex Lesions | Less effective for calcified lesions | More effective for enhancing blood flow in calcified deposits |
Conclusion
Rotablation angioplasty stands as a vital advancement in treating complex coronary artery disease, especially for patients with heavily calcified blockages. The procedure's high success rate, combined with its ability to create microscopic particles smaller than 5 microns, makes it an excellent choice when traditional angioplasty proves ineffective.
The diamond-coated burr technology offers significant advantages over conventional treatments, particularly for elderly patients with complex arterial blockages. Patients benefit from shorter recovery times compared to open-heart surgery, while doctors gain a reliable method for treating otherwise challenging cases.
Though rotablation requires specialised expertise and careful patient selection, its effectiveness in preparing vessels for stent placement and reducing complications makes it invaluable in modern cardiac care. The rotablation angioplasty continues to evolve, offering hope to individuals who previously had limited treatment options for severe coronary artery disease.
FAQs
1. What is the recovery time in rotablation angioplasty?
Recovery from rotablation angioplasty is typically quick compared to traditional open-heart surgery. Patients can walk and move about six hours after the procedure. Most individuals spend just one night in the hospital, and some return home after two days and resume work within a week.
2. Is rotablation painful?
Rotablation angioplasty is not painful for most patients. The procedure is performed under local anaesthesia that numbs the area where the catheter is inserted, usually in the groin or wrist. Patients remain awake throughout the process.
3. What are the side effects of rotablation?
Rotablation angioplasty carries several potential side effects, albeit with relatively low risk. These include:
- Arterial dissection (tear in the arterial wall)
- Perforation of the artery
- Embolisation (dislodged plaque particles causing blockages elsewhere)
- Coronary spasm (temporary narrowing causing chest pain)
- Infection at the catheter insertion site
- Allergic reactions to contrast dye
- Kidney damage
4. When do you use rotablation?
Cardiac specialists recommend rotablation angioplasty in specific circumstances:
- When plaque is particularly hard or calcified
- If blockages are so narrow that balloons cannot pass through
- When conventional balloon angioplasty fails to clear the blockage
- For patients with heavily calcified coronary arteries that resist standard treatments
ENQUIRY FORM
SELECT CATEGORIES
-
Neurosciences (16)
-
Neurology (38)
-
Neurosurgery (14)
-
Orthopaedics (48)
-
Oncology (33)
-
Obstetrics and gynecology (52)
-
Pulmonology (23)
-
Urology (20)
-
Nephrology (13)
-
Psychiatry (7)
-
Dietetics and Nutrition (111)
-
General Medicine (63)
-
Cardiac Sciences (32)
-
Vascular & Endovascular Surgery and Interventional Radiology (15)
-
Gastroenterology (46)
-
Endocrinology (23)
-
Plastic Surgery (10)
-
Critical Care Medicine (5)
-
COVID-19 (16)
-
Dermatology (16)
-
Emergency Care (1)
-
Ophthalmology (4)
-
Pediatrics (14)
-
Laparoscopic and Bariatric Surgery (8)
-
ENT (15)
-
Kidney Transplant (1)
-
Liver Transplantation and Hepatobiliary Surgery (5)
-
General Surgery (3)
-
Internal Medicine (5)
-
Medicine Information
Difference Between Heart Rate And Pulse Rate
YOU MAY ALSO LIKE
RECENT BLOGS
-
Leg Weakness: Causes, Symptoms and Treatment
9 January 2026
Read More
-

Back Pain After C-Section: Causes and Home Remedies
9 January 2026
Read More
-

Belly Button Pain (Periumbilical Pain): Causes, Treatment and When to See a Doctor
9 January 2026
Read More
-

Implantation Bleeding Vs Periods: Know the Difference
8 January 2026
Read More
-

Fainting Vs Seizure: Understand the Difference
8 January 2026
Read More
-

12 Home Remedies for Arthritis
8 January 2026
Read More
-

HeartBurn: Symptom, Causes, Risks and Treatment
8 January 2026
Read More
-

Hyperthyroidism in Men: Causes, Symptoms and Treatment
8 January 2026
Read More
Have a Question?
If you cannot find answers to your queries, please fill out the enquiry form or call the number below. We will contact you shortly.